
All clinical actions taken in a patient's record generate the creation of a clinical note. The note, therefore, includes the addition of a task, medication, allergy, etc., in addition to the text content typed, dictated, or documented in a clinical tool to summarize the consultation with the patient.
Writing and saving a clinical note
- Access the patient's record.
- Click in the Consultation reason field to start writing a note. If actions have already been taken in the patient record this day, retrieve the current clinical note.

- Document the note using the components below:
- Consultation reason
The Consultation reason field represents the title of the note. The content of this field will be visible in the Clinical notes list section when the note has been saved or completed. - Date of the note
Today's date is entered by default when a new note is opened. You can modify it if necessary to indicate the actual date of the consultation if you write your note later, or if you start it in advance. - Time of the note
The time the record is opened is registered at the opening of a new note. You can also modify it if necessary. - Note type
The following choices are available to you to associate the note with the type of consultation: Clinic visit, Phone call, or Update. - Clinical note tag
Associating tags with your note allows you to associate the subject of the consultation with the note and to filter the notes by subject thereafter. Click here for a list of available tags. 💡Configure default tags in your user profile. - Add a file
You can attach PDF, PNG and JPG files to your note.
- Consultation reason
- Document the Consultation details field:
This field is used to record the details of the consultation with the patient. To speed up writing, select a text template from those configured by your institution administrator. Voice recognition (e.g. Plume IA, Dragon Medical, Siri, etc.) can also be used. See text formating options.
The content written in this field will not immediately appear in the Clinical notes list in the record; you will have to click on the note in this section to see the content of the consultation details. - Add a clinical tool to your note such as the Framingham Score, a laboratory request, an anatomical chart or other, you can use the search bar, click on a favorite tool, or search using the available groups of clinical tools.
- Document the Consultation conclusion field:
This field allows the textual writing of the consultation summary. The content written in this field is visible in the Clinical notes list section when consulting the patient's record. - Add a confidential field (optional).
The padlock icon allows the addition of confidential information which will only be available to the author of the note in the future. Warning! Please see this article to understand its usefulness. - Regularly save the note by clicking on the Save button. When you save the note, you make sure you can find it in the patient's record later as a current note (see Completing a note below). Even if you leave the patient record, all the information entered in the note will be kept until the next backup. The note will not, however, be considered final or completed.
➡️ Text formatting in the clinical note
The Consultation details and Consultation conclusion fields support rich text, enabling you to apply formatting (bold, italics, lists, URL link, etc.) to structure your clinical notes effectively.
- Click on the icon in the top right-hand corner of the text box to display the formatting options.

- To add a symbol, press the Windows and the period (.) keys simultaniously to open the emoji & symbol panel. Navigate to the Symbols section to insert various characters.
⚠️ Limitations to keep in mind
- Adding symbols and special characters: Rich text supports the use of the following symbols: ↑ ↓ Δ ∅ → ← ± # ⊕ ⊖ @ ♀ ♂ & ≈ α β γ λ μ π Σ Ω ψ θ ϕ ρ ∑ ∞ ∝ √ ∫ ‰ ° % ′ ″ ℓ Ω Å. Any unsupported character will be replaced by an inverted question mark ' ¿ ' when saved. Contact our team to request their addition.
- Limited display of text formatting when printing in black and white: Formatting elements are supported when printing the clinical note (style, symbols, bullets and numbering, display of hyperlink URL, bold, italics, etc.). However, colored elements (colored text, highlighting) are not visible on the printout in the absence of a color printer or when sent by fax, and are then only used to facilitate reading in the EMR.
- Copy a note without the original formatting: When you copy a previous note into a new one, the copy includes the original formatting. To copy the note without the formatting, press Ctrl + Shift + V simultaneously.
The importance of documenting clinical notes
The list of clinical notes displayed when accessing the patient record is composed of notes that contain at least a consultation reason, a clinical note tag, consultation details, or a conclusion.
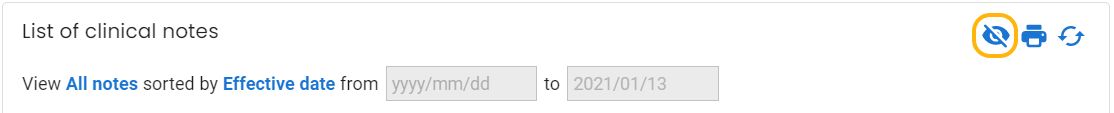
⚠️All the notes that do not have any content in one of the three fields stated above appear in what we call "the eye". For example, if you haven't filled the note during a visit, but you've entered information in the summary boxes or have filled a clinical tool, the note will appear in the eye.
Documentation of actions taken in the patient record
Note that, in the same day, each activity undertaken in the patient's record, or even outside (such as the classification of a result), is automatically recorded in the current clinical note (addition of task, allergy or problem, for example) and is presented to you in the log of the note, at the bottom of it.
Reviewing saved notes
Notes saved but not completed and notes submitted for review will be found in the Pending notes module in the left menu. To submit a note, the clinical note review functionality must be enabled in the user profile. By activating this functionality, you have the possibility to click on Send and assign a task to the caregiver who must review the note.
Completing a note
When you complete the note, you indicate that the note is final. The Complete button replaces the act of signing the note on paper.
To complete a note:
- Review the author and institution associated with the clinical note. If necessary, correct this information using the drop-down menus.

- Click on the Complete button to save and complete the note.
Complementary actions
- The Send button allows you to transmit the note via a task to another caregiver and to save the note.

- The Prebill button allows you to access your pre-billing system, if configured in your profile, to import patient information, and to save the note.